Latest analysis reveals a breakthrough in lung restore, displaying how delivering VEGFA by way of lipid nanoparticles can considerably restore broken blood vessels, akin to plumbing repairs. This technique, validated in animal fashions, presents promising insights into treating respiratory virus damages, enhancing oxygen supply, and decreasing lung irritation and scarring.
Within the human physique, the lungs and their vasculature will be likened to a constructing with an intricate plumbing system. The lungs’ blood vessels are the pipes important for transporting blood and vitamins for oxygen supply and carbon dioxide elimination. Very like how pipes can get rusty or clogged, disrupting regular water circulation, injury from respiratory viruses, like SARS-CoV-2 or influenza, can intervene with this “plumbing system.”
In a latest research, researchers seemed on the vital function of vascular endothelial cells in lung restore. Their work, printed in Science Translational Drugs, was led by Andrew Vaughan of the College of Pennsylvania’s College of Veterinary Drugs and exhibits that, by utilizing methods that ship vascular endothelial development issue alpha (VEGFA) by way of lipid nanoparticles (LNPs), that they had been capable of significantly improve modes of restore for these broken blood vessels, very similar to how plumbers patch sections of damaged pipes and add new ones.
Superior Analysis Findings
“Whereas our lab and others have beforehand proven that endothelial cells are among the many unsung heroes in repairing the lungs after viral infections just like the flu, this tells us extra concerning the story and sheds gentle on the molecular mechanisms at play,” says Vaughan, assistant professor of biomedical sciences at Penn Vet. “Right here we’ve recognized and remoted pathways concerned in repairing this tissue, delivered mRNA to endothelial cells, and consequently noticed enhanced restoration of the broken tissue. These findings trace at a extra environment friendly technique to promote lung restoration after ailments like COVID-19.”
They discovered VEGFA’s involvement on this restoration, whereas constructing on work through which they used single cell RNA sequencing to determine remodeling development issue beta receptor 2 (TGFBR2) as a serious signaling pathway. The researchers noticed that when TGFBR2 was lacking it stopped the activation of VEGFA. This lack of sign made the blood vessel cells much less capable of multiply and renew themselves, which is significant for the change of oxygen and carbon dioxide within the tiny air sacs of the lungs.
“We’d identified there was a hyperlink between these two pathways, however this motivated us to see if delivering VEGFA mRNA into endothelial cells might enhance lung restoration after disease-related harm,” says first writer Gan Zhao, a postdoctoral researcher within the Vaughan Lab.
Revolutionary Supply Strategies
The Vaughan Lab then reached out to Michael Mitchell of the College of Engineering and Utilized Science, whose lab makes a speciality of LNPs, to see if supply of this mRNA cargo can be possible.
“LNPs have been nice for vaccine supply and have confirmed extremely efficient supply autos for genetic info. However the problem right here was to get the LNPs into the bloodstream with out them heading to the liver, which is the place they have a tendency to congregate as its porous construction lends favor to substances passing from the blood into hepatic cells for filtration,” says Mitchell, an affiliate professor of bioengineering at Penn Engineering and a coauthor of the paper. “So, we needed to devise a technique to particularly goal the endothelial cells within the lungs.”
Lulu Xue, a postdoctoral researcher within the Mitchell Lab and a co-first writer of the paper, explains that they engineered the LNP to have an affinity for lung endothelial cells, this is called additional hepatic supply, going past the liver.
“We’ve seen proof within the literature suggesting it’s doable, however the methods we’d seen are made up of positively charged lipids which had been too poisonous,” Xue says. “This led me to creating an ionizable lipid that’s not positively charged when it enters the bloodstream however will get charged when it will get to the endothelial cells, thereby releasing the mRNA.”
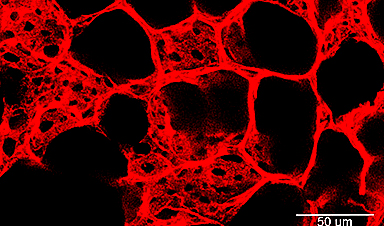
Their LNPs proved efficient in delivering VEGFA into endothelial cells and in consequence, the researchers noticed a marked enchancment in vascular restoration of their animal fashions. Inside the animal fashions, the researchers noticed improved oxygen ranges, and in some, the therapy helped them get better their weight higher than the management group. These handled mice additionally had much less lung irritation, proven by decrease ranges of sure markers of their lung fluid, and their lungs confirmed much less injury and scarring, with extra wholesome blood vessels.
“Though we went in hoping for this final result, it was an actual thrill to see how efficient, secure, and effectively this all panned out, so we’re wanting ahead to testing this supply platform for different cell varieties within the lung, and it is going to be necessary to guage whether or not TGFB signaling is necessary in different harm contexts together with persistent situations like emphysema and COPD,” Vaughan says. “With this proof-of-concept being effectively validated, we’re positive that we’ll pave the way in which for brand spanking new mRNA-based methods for treating lung harm.”
Reference: “TGF-βR2 signaling coordinates pulmonary vascular restore after viral harm in mice and human tissue” by Gan Zhao, Lulu Xue, Aaron I. Weiner, Ningqiang Gong, Stephanie Adams-Tzivelekidis, Joanna Wong, Maria E. Gentile, Ana N. Nottingham, Maria C. Basil, Susan M. Lin, Terren Ok. Niethamer, Joshua M. Diamond, Christian A. Bermudez, Edward Cantu, Xuexiang Han, Yaqi Cao, Mohamad-Gabriel Alameh, Drew Weissman, Edward E. Morrisey, Michael J. Mitchell and Andrew E. Vaughan, 31 January 2024, Science Translational Drugs.
DOI: 10.1126/scitranslmed.adg6229
Andrew Vaughan is an assistant professor within the Division of Biomedical Sciences on the College of Pennsylvania College of Veterinary Drugs.
Michael Mitchell is an affiliate professor within the Division of Bioengineering within the College of Engineering and Utilized Science and the director of the Lipid Nanoparticle Synthesis Core on the Penn Institute for RNA Innovation on the College of Pennsylvania.
Gan Zhao is a postdoctoral researcher within the Vaughn Lab at Penn Vet.
Lulu Xue is a postdoctoral researcher within the Mitchell Lab at Penn Engineering.
Different authors embrace Stephanie Adams-Tzivelekidis, Maria E. Gentile, Aaron I. Weiner, and Joanna Wong from Penn Vet; Ningqiang Gong and Xuexiang Han from Penn Engineering; and Mohamad-Gabriel Alameh, Maria C. Basil, Christian A. Bermudez, Edward Cantu, Yaqi Cao, Joshua M. Diamond, Susan M. Lin, Edward E. Morrisey, Terren Ok. Niethamer, Ana N. Nottingham, and Drew Weissman within the Perelman College of Drugs at Penn.
This work was supported by the Nationwide Institutes of Well being (grants R01HL153539 and R01HL164350 and award DP2 TR002776, the Margaret Q. Landenberger Basis, a Burroughs Wellcome Fund Profession Award on the Scientific Interface; and the Nationwide Science Basis (Award CBET-2145491).