Scientists have uncovered a essential piece of the puzzle in autoimmune illnesses: a protein that helps launch immune response molecules.
By learning an ultra-rare situation, researchers recognized ArfGAP2 as a key participant in immune overactivity. Blocking it in mice prevented extreme tissue harm, opening the door to potential therapies for a variety of immune-related illnesses, together with COVID-19 and Alzheimer’s.
Unraveling the Thriller of Autoimmune Triggers
Autoimmune illnesses have an effect on over 15 million individuals within the U.S. They happen when the physique errors its personal wholesome tissues for threats, triggering immune “false alarms.” This results in immune cells attacking the physique as a substitute of dangerous invaders. Whereas scientists have lengthy understood how these false alarms start, the following step, how the immune system mobilizes its assault, has remained unclear.
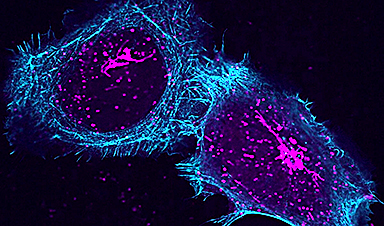
Now, researchers at Washington College Faculty of Medication in St. Louis and the Perelman Faculty of Medication on the College of Pennsylvania have found an important piece of that puzzle. They’ve recognized a beforehand unknown protein that helps set off the discharge of infection-fighting molecules from cells. This protein seems to play a key function in each regular immune responses and dangerous overreactions.
Due to its central function, the protein could possibly be a promising goal for creating therapies to deal with autoimmune illnesses and different situations linked to immune system overactivity. The findings have been printed on-line on February 12 in Cell, and appeared in print on March 20.
A Breakthrough in Uncommon Illness Analysis
The group of researchers, co-led by Jonathan Miner, MD, PhD, an affiliate professor of Rheumatology and Microbiology and a member of Penn’s Colter Middle for Autoimmunity, and David Kast, PhD, an assistant professor within the Division of Cell Biology & Physiology at WashU Medication, made the invention by learning a uncommon autoimmune illness referred to as STING-associated vasculopathy with onset in infancy (SAVI). The situation is extraordinarily uncommon, occurring in one in all each 1 million births. It results in the immune response attacking tissues within the lungs and limbs of sufferers, typically leading to demise earlier than maturity.
Finding out uncommon illnesses the place the basis reason for the illness is attributable to a single mutation cannot solely reveal the organic function of the affected gene and the disease-causing disruptions it incites, but in addition present perception into more-common situations.
The Position of STING in Autoimmune Assaults
SAVI is attributable to adjustments to a protein in cells referred to as STING, which ordinarily acts as a molecular watchdog that responds to the presence of viral DNA by activating the part of the cell that generates immune proteins. These immune proteins are then launched from the cell to sign to the physique’s immune system of the necessity to assault the viral invaders, and the place within the physique the immune cells must go. In SAVI, STING is overactive, triggering fixed immune exercise that finally damages wholesome tissue.
Along with signaling the cell to make the immune-response proteins, referred to as cytokines, the researchers found that STING additionally has a novel function in releasing these proteins from the place they’re made within the cell. How that launch course of labored was unknown, however discovering a method to management it could possibly be a promising avenue for treating SAVI in addition to different autoimmune problems.
Discovering ArfGAP2: The Lacking Piece
Utilizing immune cells that have been delicate to the disease-causing mutations in STING, the group carried out a display to determine proteins that prevented this sensitivity. One protein, ArfGAP2, stood out, because it appeared to be strongly linked to the ultimate step when the immune response proteins get launched.
The group additional validated this discovering in SAVI cells that didn’t produce ArfGAP2. With out it, STING couldn’t drive the discharge the immune proteins.
“It’s like a prepare station and ArfGAP2 is performing because the conductor, directing which molecules are to be shipped out,” stated Kast. “If STING and ArfGAP2 aren’t working collectively, the trains are stopped.”
The group reasoned that stopping the unending “trains” in SAVI’s fixed immune response could possibly be a way of treating the uncommon illness.
A Path Towards New Remedies
The group examined that concept in a mouse that was genetically modified to have SAVI, however didn’t produce the ArfGAP2 protein. They discovered that the lung- and limb-destroying immune response typical of the illness didn’t happen, which confirmed that if the protein could possibly be neutralized, the overactive immune response could possibly be turned off.
Miner, who initiated the challenge when he was at WashU Medication, stated that it’s a promising goal for different situations that equally result in extra immune proteins of the identical sort. This might embody the “cytokine storms” attribute of COVID-19 or the mind irritation linked to immune responses in Alzheimer’s illness.
Uncommon Ailments Unlocking Broader Medical Insights
“Ailments like SAVI which might be tremendous uncommon can present beneficial insights,” stated Miner, “as a result of should you can work out how a uncommon illness mutation is working, you be taught one thing in regards to the regular proteins that each one of us have. Then out of the blue you’ve opened the doorways to all these new avenues of potential therapies for a lot of, many alternative lessons of illnesses.”
Reference: “ArfGAP2 promotes STING proton channel exercise, cytokine transit, and autoinflammation” by Subhajit Poddar, Samuel D. Chauvin, Christopher H. Archer, Wei Qian, Jean A. Castillo-Badillo, Xin Yin, W. Miguel Disbennett, Cathrine A. Miner, Joe A. Holley, Teresa V. Naismith, W. Alexander Stinson, Xiaochao Wei, Yue Ning, Jiayuan Fu, Trini A. Ochoa, Nehalee Surve, Shivam A. Zaver, Kimberly A. Wodzanowski, Katherine R. Balka, Rajan Venkatraman, Canyu Liu, Kelly Rome, Will Bailis, Yoko Shiba, Sara Cherry, Sunny Shin, Clay F. Semenkovich, Dominic De Nardo, Sunnie Yoh, Elisha D.O. Roberson, Sumit Ok. Chanda, David J. Kast and Jonathan J. Miner, 12 February 2025, Cell.
DOI: 10.1016/j.cell.2025.01.027
This work was supported by NIH grant numbers R01 AI143982, R01 436 NS131480, R01 GM136925, in addition to funding from the Colton Middle for Autoimmunity and the Clayco Basis to J.J.M. The content material is solely the duty of the authors and doesn’t essentially signify the official views of the Nationwide Institutes of Well being (NIH).